Caso clÃnico y revisión
Angioplasty in heavily calcified coronary lesions. Early experience with coronary intravascular lithotripsy
Sebastián Peralta, Carlos Fernández Pereira, Carla Agatiello, Juan Pablo De Brahi, Juan Mieres, Horacio Medina de Chazal, MartÃn Bodoira, Marcelo Bettinotti
Revista Argentina de Cardioangiología Intervencionista 2021;(2): 0088-0092 | Doi: 10.30567/RACI/20212/0088-0092
The presence of heavily calcified coronary lesions has been our main public enemy for some time now because it affects the results of the angioplasty by initially preventing balloon crossing, complicating the proper passage of the drug from the surface of the stent to the vascular wall, and reducing stent expansion and apposition. These effects keep a direct correlation with the short and long-term progression of these patients. Different devices have been created like noncompliant balloons, cutting balloons, rotational and orbital atherectomy, and intracoronary laser with different crossover profiles and results. A new alternative is coronary lithotripsy, capable of achieving the circumferential fracture of calcified plaques without changing the flow after the procedure. The early outcomes of cases performed with the Shockwave 2 C IVL system are presented here.
Palabras clave: coronary stenosis, lithotripsy, vascular calcification.
La presencia de lesiones coronarias severamente calcificadas ha sido nuestro principal enemigo porque afecta los resultados de la angioplastia al impedir el cruce inicial de los balones, no permite el adecuado paso del fármaco de la superficie del stent a la pared vascular, reduce la expansión y la aposición del stent. Estos efectos tienen una directa relación con la evolucion a corto y largo plazo de estos pacientes. Se han ideado diferentes dispositivos como balones no complacientes, balones con corte, aterectomía rotacional (AR) y orbitaria, láser intracoronario con diferentes perfiles de cruce y resultados. Una nueva alternativa es la litotricia coronaria, que logra la fractura circunferencial de las placas calcificadas, sin modificar el flujo luego del procedimiento. Se presentan los resultados iniciales de casos realizados con Shockwave 2 C IVL (Shockwave Medical, Fremont, California).
Keywords: estenosis coronaria, litotricia, calcificación vascular.
Los autores declaran no poseer conflictos de intereses.
Fuente de información Colegio Argentino de Cardioangiólogos Intervencionistas. Para solicitudes de reimpresión a Revista Argentina de CardioangiologÃa intervencionista hacer click aquí.
Recibido 2021-06-03 | Aceptado 2021-06-14 | Publicado

Esta obra está bajo una Licencia Creative Commons Atribución-NoComercial-SinDerivar 4.0 Internacional.



Introduction
Heavily calcified coronary lesions complicate the advancement of balloons and a proper stent expansion and apposition. Different devices have come up today for the management of this type of lesions. High-pressure noncompliant balloons are initially used to dilate areas with fewer calcification with the possibility of generating dissections but without ever changing the plaque calcification. Special balloons like the scoring balloon and the cutting balloon have the same drawbacks regarding crossing difficulties due to the high profile of these devices. In moderate calcifications, another device that still remains unavailable in our country has been used: the intracoronary laser. It can be useful in unexpanded coronary stents. Other devices like rotational and orbital atherectomy are highly effective facilitating the crossing of the lesion. Still, there are instances that their mechanism of action can cause slow-flow or no reflow in the thrombotic lesion setting. Intravascular lithotripsy (IVL) is a new technique based on an already established therapeutic strategy for the management of kidney stones where multiple lithotripsy emitters mounted over a catheter deliver localized pulsatile sonic pressure waves to circumferentiallt modify vascular calcium and break down the calcium deposits of the tunica intima and tunica media. We present an early series of patients treated successfully in different centers with the Shockwave IVL system.
Clinical case #1
This is the case of a 71-year-old male patient with cardiovascular risk factors: arterial hypertension, non-insulin-dependent diabetes mellitus type 2, smoker of 60 packs/year, and overweight. Past cardiovascular medical history: acute myocardial infarction in 2005. Patient on medical therapy.
Triple vessel disease: myocardial revascularization surgery (2011 – LIMA to LAD; RADIAL graft to the LV side of the CXI, and VG to posterior descending branch of RCA). Functional class (FC) II stable chronic angina of 6-month evolution. Past medical history: appendectomy (at 16), vesical polypectomy of benign pathology, tear of the Achilles tendon repaired surgically back in 2010. Usual medication: acetylsalicylic acid, 100 mg/day; bisoprolol, 5 mg/12 hours. Rosuvastatin 10 mg/day; enalapril, 10 mg/12 hours; omeprazole, 20 mg/day; metformin, 850/12 hours, Lantus insulin 20 IU for subcutaneous use. On December 30, 2020, the patient was hospitalized with signs of left upper extremity arterial ischemia, probable paroxysmal atrial fibrillation, and FC IV angina pectoris. On January 1, 2021, a cine coronary arteriography and an arteriogram of the left upper extremity revealed: left main coronary artery without significant findings; left anterior descending coronary artery occluded in its proximal portion (70%) and middle third (100%); a heavily calcified left circumflex artery occluded in its proximal third (90%); right coronary artery occluded in its middle third; patent left internal mammary artery graft to left anterior descending coronary artery; radial graft to the LV side of patent left circumflex artery. Venous graft to posterior descending branch of patent right coronary artery. Unsuccessful percutaneous coronary intervention (PCI) approach to left circumflex artery. Occluded humeral artery treated with a Fogarty catheter. The echocardiogram shows an EF = 44%. Exercise-rest same-day SPECT protocol (February 2021): Inferior and inferior-lateral necrosis. Lateroapical and apical ischemia. Severely depressed ejection fraction (EF) after exercise. February 23, 2021.
Scheduled PCI: calcified lesion with Rotablator and then coronary lithotripsy (RotaTripsy) followed by the implantation of 1 DES into the left circumflex artery. The patient remains asymptomatic at the 3-month follow-up.
Clinical case #2
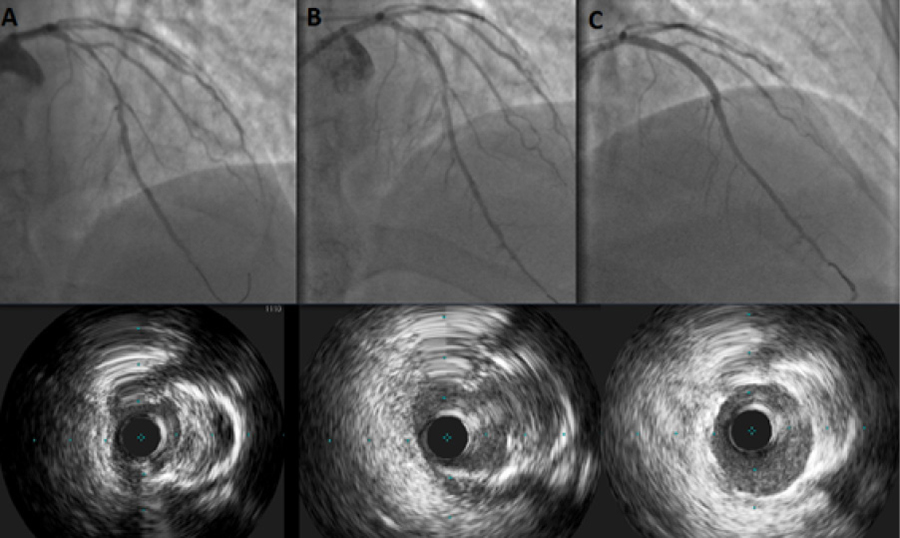
This is the case of a 60-year-old male patient with cardiovascular risk factors: arterial hypertension, and type II diabetes. Angina of 2-month evolution. Current medication: aspirin, 100 mg; clopidogrel, 75 mg; rosuvastatin, 20 mg; valsartan, 160 mg; bisoprolol, 5 mg, and omeprazole, 20 mg. The myocardial perfusion imaging (MPI) with single-photon emission computed tomography (SPECT) revealed signs of ischemia of the anterior wall at 7 METs, 18 000/double product (ITT). The PCI was performed on the heavily calcified left anterior descending coronary artery via right radial approach. A XBU 3.5 6-Fr guide catheter was inserted with IVUS Philips Refinity guidance. Dilatation with the Shockwave device was performed followed by DES implantation and the corresponding follow-up (Figure 1). The patient remained asymptomatic at the 3-month follow-up.
Clinical case #3
This is the case of an 80-year-old male patient with cardiovascular risk factors: former smoker who quit smoking quite a few years ago. Past medical history of complete left bundle branch block. Current disease: FC I-II dyspnea of 1-year evolution. No signs of angina. The outpatient physical examination with SPECT revealed an impaired ejection fraction. A cine coronary arteriography was performed. Back in March 2020 the CCG had already been scheduled but never got to be performed. Mild ventricular dysfunction described in 2020. Transthoracic echocardiogram findings: severe left ventricular dysfunction, septal dyskinesia, moderate aortic regurgitation, moderate mitral regurgitation, aortic root diameter, 3.9 as seen on the CCG. Atherosclerotic coronary artery disease with compromise of left anterior descending coronary artery with significant ostial/proximal stenosis with heavily calcified plaque spreading from the distal third of the left main coronary artery (Figure 2A). Dominant left circumflex artery with irregularities. Right coronary artery: irregularities. It is decided to perform a PCI with IVL (Shockwave). Procedure: right radial puncture with a 7-Fr catheter is performed followed by the infusion of 7500 IU of heparin. 1) The intravascular ultrasound (IVUS) performed reveals a heavily calcified atherosclerotic plaque (180°) causing significant luminal stenosis. 2) Predilatation with intravascular lithotripsy (Shockwave) is attempted with good angiographic outcomes (40 pulses). The correct predilatation and fracture of the calcium deposit is confirmed on the IVUS (Figure 2B). 3) Afterwards, a PCI is performed on the ostial/proximal region of the left anterior descending coronary artery and one 4.0 mm x 18 mm drug-eluting stent is implanted. Postdilatation with a 5.0 mm noncompliant balloon is attempted. The correct stent expansion and apposition is confirmed on the IVUS (Figure 2C). NOTE: a total of 120 mL of low osmolar iodinated contrast were used. The patient remained asymptomatic at the follow-up.
Clinical case #4
This is the case of an 83-year-old female patient who presents with oppressive precordial pain (9/10 intensity) radiating to her left arm of 2-hour evolution with accompanying symptoms of profuse sweating, nausea, and vomiting. Cardiovascular risk factors: age, arterial hypertension, dyslipidemia. Past medical history: depression, lumbar spinal fusion, and bilateral total hip arthroplasty. Current medication: irbesartan, 12.5 mg; paroxetine, 20 mg, and simvastatin, 20 mg. The patient had no fever at admission, and 90 bpm. Blood pressure levels: 140/85. Systolic heart murmurs in mitral area radiating to the armpit with pulmonary middle crackles. ECG findings: atrial fibrillation, negative T waves in the anterior wall. Lab parameters: elevated troponin levels. Early diagnosis of non-ST-segment elevation acute coronary syndrome, Grace risk score 138, and TIMI grade-2 flow. The patient is administered clopidogrel, NTG, furosemide, and atorvastatin, and pain intensity goes down to 4/10. Echocardiogram findings: severe anterior hypokinesis at the anteroapical and apical segments, severe lateral hypokinesis. Moderate eccentric mitral regurgitation jet. EF = 48%. The cine coronary arteriography performed confirmed the presence of a calcified moderate ostial lesion of the right coronary artery, ostium, and left main coronary artery without lesions. Proximal severe lesion at left circumflex artery level. Heavily calcified left anterior descending coronary artery in its middle third with a 95% lesion compromising the origin of the diagonal artery with proximal severe lesion and occlusion receiving collateral circulation from the left anterior descending coronary artery. SYNTAX score = 40, and ERACI score = 32. A balloon angioplasty is performed with 1.25 mm, 1.5 mm, 2.0 mm, and 2.5 mm high-pressure balloons that fail to achieve plaque dilatation (Figure 3). Therefore, an IVL is performed with new gradual dilatations emitting a total of 80 pulses with a 2.5 mm x 12 mm Shockwave c2 IVL device (Shockwave Medical, Fremont, CA, United States) achieving a good diameter of dilatation without dissection images and a proper blood flow. Afterwards, 2 overlapping BMSs were implanted at high atmospheres of pressure (Figure 4). Finally, a PCI is performed on the left circumflex artery with 1 BMS implantation using the ORCA Colchicine 0.5 mg protocol. The patient remained asymptomatic for angor pectoris and dyspnea at the 2-month follow-up.
Discussion
The use of imaging modalities in calcified lesions is crucial to determine the type of device that should be used for treatment purposes. Fluoroscopy underestimates the presence of endoluminal calcium. Also, the calcium detected on the fluoroscopy is sometimes found at the adventitia-tunica media interface (Mönckeberg’s arteriosclerosis). IVUS is the most reliable diagnostic imaging modality for the detection of endoluminal and deep calcium. However, the border of endoluminal calcium hides in its shadow the actual mass of calcium in the vessel wall. Optical coherence tomography (OCT) has a limited capacity of penetration but high sensitivity and specificity rates to see images of superficial calcium and assess the posterior region of the calcified plaque being able to measure the entire actual calcified mass. Unfortunately, the last 2 imaging modalities described are not very much used due to their cost and the fact that they are not covered by most patients’ health insurances. Maybe in the coming future, the multislice computed tomography (MTSC) will be used to define de load and show the interventional cardiology the plan he should follow for the management of these calcified plaques (rotational atherectomy, orbital atherectomy, lithotripsy).5,6
After experimental in vitro studies, in December 2015 the DISRUPT CAD I trial was started1 including 60 patients from 7 hospitals from 5 different countries. The median stenosis rate was 72.5% and the average lesion length, 18.2 mm, and severe calcification was present in all the patients. The IVL was feasible and facilitated stent implantation in all the patients, brought the rate of stenosis down to 12.2% with an acute gain of 1.7 mm, a 95% rate of clinical success, and no MACE at the 30-day follow-up (rate of 95%). No dissections, slow flow/no reflow, embolization or perforations were reported. The rate of MACE at the 6-month follow-up was 8.3%.
This first study describes the effect mechanism as seen on the optical coherence tomography (OCT) in heavily calcified lesions that would later be implanted with a stent,2 with localized disruption as a way to prepare the vessel. It is an early sub-analysis of 31 patients from the DISRUPT CAD I trial. The lithotripsy broke calcium down in 43% of the lesions. The rate of calcium breaking increased in the most heavily calcified plaques. The mean gain of the acute area was 2.1 mm2, but it went up even more with stent implantation achieving minimal stent areas of 5.94 mm2 +- 1.98 mm2. Deep dissections as part of the effect of the angioplasty occurred in 13% of the cases that were successfully treated with stent implantation without acute occlusions, slow flow/no-reflow or perforations ever occurring.
In order to confirm the safety and efficacy profile of IVL, the DISRUPT CAD II was conducted.4 It is a prospective, multicenter, single-arm study conducted in 15 hospitals from 9 different countries. An OCT substudy was conducted to assess the mechanism of action of IVL. Independent central imaging core labs adjudicated the angiography and the optical coherence tomography, and an independent clinical events committee adjudicated the major adverse cardiovascular events. A total of 120 patients were recruited. IVL catheter implantation was successful in all the patients. The post-IVL angiographic acute luminal gain was 0.83 mm ± 0.47 mm, and residual stenosis, 32.7% ± 10.4% (that went down even more to 7.8% ± 7.1% after drug-eluting stent implantation). The main assessment endpoint consisting of 7 non-Q wave myocardial infarctions was met by 5.8% of the patients. No acute occlusions, slow flow, no-reflow or perforations were reported. The breaking of calcium deposits was identified in 78.7% of the lesions with 3.4 ± 2.6 fractures per lesion of an average 5.5 mm ± 5.0 mm in length.
These studies allowed us to start gaining experience in cases from numerous centers10, 11, 12,13,14 thanks to their numerous case reports and editorials,5,8,21,22 which extended the indications not only to de novo lesions, but also to the use of 5-Fr introducer sheaths via radial approach.15 This added to the indications for underexpansions of previously implanted stents and to the recanalization procedure suggested to treat chronic total coronary occlusions16 with large amounts of calcium.
An unexpanded stent in a heavily calcified coronary lesion is a common complication that can go on for years. It is associated with long-term failure and a poor evolution. Treatment with intracoronary lithotripsy may be an option here. In a case of an unexpanded coronary stent implanted 11 years ago, the optical coherence tomography revealed the mechanism of stent underexpansion by showing the presence of calcium deposits underneath the old struts.27 The IVL breaks down the calcium underneath the stent struts changing its geometry from an elliptical to a round shape. Consequently, this transmits the old stent radial strength even better with the corresponding balloon dilatation.28,29
Another strategy that has joined the therapeutic armamentarium for the management of calcified lesions is combining rotational atherectomy (RA) and IVL. RA and IVL techniques can complement each other.20, 25 The RA allows us to treat the calcium deposits of the tunica intima and cross balloons or stents through heavily calcified lesions; however, it may not be enough to achieve the proper expansion of these devices in the presence of deep circumferential calcium deposits. The IVL is a useful tool for the management of deep nondilatable calcium plaques. Nonetheless, it is very difficult to access severe and diffuse lesions due to their crossing profile. The combination of both techniques (called RotaTripsy) can be useful for the percutaneous management of heavily calcified lesions.
Thanks to the crossing profile of the IVL balloon, different accessories can be used to reach the target plaque. An early case of intracoronary lithotripsy used an extension catheter7 to treat a heavily calcified and angulated left circumflex artery. Although the lithotripsy balloon available today is relatively large, the exchange extension catheter adapted it quite easily facilitating its placement. This case showed the utility of this combination of devices for patients with complex coronary anatomies.
We should mention that the IVL is a new technique that is still associated with some unwanted effects.9 As a matter of fact, the IVL can cause ventricular ectopy.17, 18, 24 Also, asynchronous cardiac pacing was described in a retrospective review of cases of coronary IVL performed in Belfast, Northern Ireland3 with an incidence rate of ventricular capture of 77.8%. Heart rate > 65 bpm was identified as the only independent predictor of a higher risk of IVL-induced ventricular capture. However, no major adverse clinical events associated with this phenomenon in this series were reported. Another possible unwanted side effect on the conduction system that may occur during IVL is atrial fibrillation.23 In the case reported reversion to sinus rhythm occurred a few hours after the procedure allowing an early hospital discharge. Another unwanted effect due to calcified plaques is the rupture of the IVL balloon.19 This phenomenon is similar to other balloons that also rupture due to calcium deposits.
The most recent study on IVLis the DISRUPT CAD III trial.30 It is a prospective, multicenter, single-arm study designed to approve coronary IVL. The main safety endpoint was the lack of MACE (a composite of death, myocardial infarction or target vessel revascularization at the 30-day follow-up). The main efficacy endpoint was procedural success. Both assessment endpoints were compared using a pre-established performance goal (PG). The mechanism of calcium modification was assessed on an optical coherence tomography (OCT) substudy. A total of 431 patients from 47 centers from 4 different countries were included. The primary safety endpoint at 30 days was the lack of MACE in 92.2% of the cases; The primary efficacy endpoint was procedural success in 92.4% of the cases. The mean length of the calcified segment was 47.9 mm + -18.8 mm, the calcium angle was 292.5º ± 76.5º, and calcium thickness was 0.96 mm + -0.25 mm at the most heavily calcified site. The OCT revealed the presence of fractures of multiplane and longitudinal calcium after the IVL in 67.4% of the lesions. The minimal stent area went from 6.5 mm2 to 2.1 mm2 and was similar whether fractures were seen on the OCT or not.
The IVL is a promising technique to overcome the problems associated with heavily calcified non-dilatable de novo lesions. Also, it helps in cases of inadequate stent expansion by eventually modifying the plaque and achieving successful stent implantations too as intravascular imaging confirm.26
Conclusions
In this early series of patients with heavily calcified lesions, the coronary intravascular lithotripsy facilitated a proper dilatation prior to stent implantation without any adverse events reported during the procedure or at the follow-up
-
Brinton TJ, Ali Z, Hill J, et al. Feasibility of Shockwave Coronary Intravascular Lithotripsy for the Treatment of Calcified Coronary Stenoses: First Description. Circulation 2019. 139:834-6.
-
Rheude T, Rai H, Richardt G, et al. Super High-Pressure Balloon versus Scoring Balloon to Prepare Severely Calcified Coronary Lesions: The ISAR-CALC Randomized Trial. EuroIntervention. 2020 Dec 1:EIJ-D-20-01000.
-
Zhang XY, Tang Z, Zeng YP, Nie SP. Comparison of Lacrosse Non-Slip Elements and Cutting Balloons in Treating Calcified Coronary Lesions: a Retrospective, Single-Blind Randomized Controlled Study. Adv Ther. 2019 Nov;36(11):3147-53.
-
Bilodeau L, Fretz EB, Taeymans Y, Koolen J, Taylor K, Hilton DJ. Novel use of a high-energy excimer laser catheter for calcified and complex coronary artery lesions. Catheter Cardiovasc Interv. 2004 Jun;62(2):155-61.
-
Iannopollo G, Gallo F, Mangieri A, et al. Tips and Tricks for Rotational Atherectomy. J Invasive Cardiol. 2019 Dec;31(12):E376-E383.
-
Chambers JW, Feldman RL, Himmelstein SI, et al. Pivotal trial to evaluate the safety and efficacy of the orbital atherectomy system in treating de novo, severely calcified coronary lesions (ORBIT II). JACC Cardiovasc Interv. 2014 May;7(5):510-8.
-
Ali ZA, Brinton TJ, Hill JM, et al. Optical Coherence Tomography Characterization of Coronary Lithoplasty for Treatment of Calcified Lesions: First Description. JACC Cardiovasc Imaging. 2017 Aug;10(8):897-906.
-
Kassimis G, Raina T, Kontogiannis N, et al. How Should We Treat Heavily Calcified Coronary Artery Disease in Contemporary Practice? From Atherectomy to Intravascular Lithotripsy. Cardiovasc Revasc Med. 2019 Dec;20(12):1172-83.
-
Brinton TJ, Ali ZA, Hill JM, et al. Feasibility of Shockwave Coronary Intravascular Lithotripsy for the Treatment of Calcified Coronary Stenoses. Circulation. 2019 Feb 5;139(6):834-6.
-
Ali ZA, Brinton TJ, Hill JM, et al. Optical Coherence Tomography Characterization of Coronary Lithoplasty for Treatment of Calcified Lesions: First Description. JACC Cardiovasc Imaging. 2017 Aug;10(8):897-906.
-
Ali ZA, Nef H, Escaned J, et al. Safety and Effectiveness of Coronary Intravascular Lithotripsy for Treatment of Severely Calcified Coronary Stenoses: The Disrupt CAD II Study. Circ Cardiovasc Interv. 2019 Oct;12(10):e008434.
-
Sgueglia GA, Gioffrè G, Piccioni F, Gaspardone A. Slender distal radial five French coronary shockwave lithotripsy. Catheter Cardiovasc Interv. 2019 Sep 1;94(3):395-39.
-
Azzalini L, Bellini B, Montorfano M, Carlino M. Intravascular lithotripsy in chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2019 Dec 6;15(11):e1025-6.
-
Demarchi A, Ugo F, Chiara C, Rametta F. Very late stent expansion with intracoronary lithotripsy: a case report. Eur Heart J 2020;4:1-4.
-
Ielasi A, Loffi M, De Blasio G, Tespili M. “Rota-Tripsy”: A Successful Combined Approach for the Treatment of a Long and Heavily Calcified Coronary Lesion. Cardiovasc Revasc Med. 2020 Nov;21(11S):152-154. doi: 10.1016/j.carrev.2019.12.023. Epub 2019 Dec 18. PMID: 31883981.
-
Warisawa T, Goto S, Salazar CH, Akashi YJ, Escaned J. Safety and Feasibility of Coronary Lithotripsy Supported by Guide Extension Catheter for the Treatment of Calcified Lesion in Angulated Vessel. Cardiovasc Revasc Med 2019 Nov;20(11S):6-8.
-
Wilson SJ, Spratt JC, Hill J, et al. Incidence of “shocktopics” and asynchronous cardiac pacing in patients undergoing coronary intravascular lithotripsy. EuroIntervention. 2020 Mar 20;15(16):1429-35.
-
Curtis E, Khan A, El-Jack S, Glenie T. Precipitation of de novo atrial fibrillation during Shockwave Intravascular Lithotripsy® after pacing capture during the treatment of proximal right coronary artery disease: a case report. Eur Heart J Case Rep 2019;3(4):1-4.
-
Soriano F, Veas N, Piccinelli E, Oreglia J. Coronary dissection due to intravascular lithoplasty balloon rupture. EuroIntervention. 2019 9;15(6):e558-9.
-
Hill JM, Kereiakes DJ, Shlofmitz RA, et al.; Disrupt CAD III Investigators. Intravascular Lithotripsy for Treatment of Severely Calcified Coronary Artery Disease. J Am Coll Cardiol. 2020 Dec 1;76(22):2635-2646. doi: 10.1016/j.jacc.2020.09.603. Epub 2020 Oct 15. PMID: 33069849.
-
La Manna A, D’Agosta G, Venuti G, Tamburino C. Cracking the Plaque With Coronary Lithotripsy: Mechanistic Insights From Optical Coherence Tomography. J Invasive Cardiol. 2020 Jan;32(1):E14. PMID: 31893507.
Sebastián Peralta
Servicio de Hemodinamia. Sanatorio Güemes. CABA. Argentina.
Carlos Fernández Pereira
Centro de Estudios en CardiologÃa Intervencionista. (CECI).CABA. Servicio de Hemodinamia. Sanatorio Otamendi. CABA. Argentina.
Carla Agatiello
Servicio de Hemodinamia. Hospital Italiano. CABA. Argentina.
Juan Pablo De Brahi
Servicio de Hemodinamia. Sanatorio Trinidad Mitre .CABA. Argentina.
Juan Mieres
Centro de Estudios en CardiologÃa Intervencionista. (CECI).CABA. Argentina.
Horacio Medina de Chazal
Servicio de Hemodinamia. Hospital Italiano. CABA. Argentina.
MartÃn Bodoira
Servicio de Hemodinamia. Sanatorio Trinidad Mitre .CABA. Argentina.
Marcelo Bettinotti
Servicio de Hemodinamia. Sanatorio Güemes. CABA. Argentina.
Autor correspondencia
Carlos Fernández Pereira
Centro de Estudios en CardiologÃa Intervencionista. (CECI).CABA. Servicio de Hemodinamia. Sanatorio Otamendi. CABA. Argentina.
Correo electrónico: cfernandezpereira@centroceci.com.ar.
Para descargar el PDF del artículo
Angioplasty in heavily calcified coronary lesions. Early experience with coronary intravascular lithotripsy
![]() Haga click aquí
Haga click aquí
Para descargar el PDF de la revista completa
Revista Argentina de CardioangiologÃa intervencionista, Volumen Año 2021 2
Revista Argentina de CardioangiologÃa intervencionista
Issue # 2 | Volumen
11 | Año 2021
SOLACI/CACI Congress: a long journe...
Alfredo E RodrÃguez
Repetitive and outpatient infusions...
Florencia Noutary y cols.
Neutrophil-to-lymphocyte ratio to p...
Suilbert RodrÃguez Blanco y cols.
Angioplasty in heavily calcified co...
Sebastián Peralta y cols.
Traumatic arteriovenous fistula. En...
Esteban MartÃn Quarchioni y cols.
Cardiac hamartoma: role of endomyoc...
José MarÃa Milanesi y cols.
Coronary stenting in the right vent...
Jorge Gómez y cols.
Endovascular therapeutic options fo...
Daniela Battisti y cols.
The importance of cardiovascular in...
Diego Grinfeld
Etiquetas
coronary stenosis, lithotripsy, vascular calcification
Tags
estenosis coronaria, litotricia, calcificación vascular
Angioplasty in heavily calcified coronary lesions. Early experience with coronary intravascular lithotripsy
Autores
Sebastián Peralta, Carlos Fernández Pereira, Carla Agatiello, Juan Pablo De Brahi, Juan Mieres, Horacio Medina de Chazal, MartÃn Bodoira, Marcelo Bettinotti
Publicación
Revista Argentina de CardioangiologÃa intervencionista
Editor
Colegio Argentino de Cardioangiólogos Intervencionistas
Fecha de publicación
2021-06-30
Registro de propiedad intelectual
© Colegio Argentino de Cardioangiólogos Intervencionistas










